January is National Cervical Cancer Awareness Month
In our previous cervical cancer awareness post, we covered the causes:
https://bloom-obgyn.com/january-is-national-cervical-cancer-awareness-month/
And now….
CERVICAL CANCER: SCREENING & DIAGNOSIS

George Papanicolaou was a pioneer in cytopathology and creator of the Papanicolaou test or “Pap smear”. He first published a study in 1928 outlining the different microscopic cellular structures of normal female reproductive cells compared to malignant or cancer cells. Ongoing research and study resulted in a landmark publication in 1943 that revolutionized the early detection of cervical cancer and, thus, the Pap test. It led to a 70% reduction in cervical cancer deaths and is still one of our current screening methods. The other principal screening tool for cervical cancer is a Human Papillomavirus or HPV test on the cells of the cervix.
How is a Pap test different from HPV screening?
A Pap test evaluates the actual cells on your cervix. During a pelvic exam, a brush is used to collect these cells which are then sent to a lab for review. A Pathologist examines the cells under a microscope and issues a report with their findings – either normal cells or abnormal cells with different levels of abnormality.
The HPV screen can be done at the same time as a Pap test (or on its own), but the technology is different. The lab looks for DNA from different HPV strains in those same cells as your Pap test. The presence of DNA indicates an infection with the virus. When these tests are run together, we call that “co-testing” and this is the common recommendation for cervical cancer screening.
When does cervical cancer screening start? And how often is it done?
Cervical cancer is very rare under age 21 and the current recommendation is to start screening for cervical cancer at that age. Co-testing typically starts at 30 years old. The frequency of testing varies. Your personal history, current medical concerns and the results of previous Pap tests and HPV screens determine the schedule. For instance, recommendations range from every 6 months to every 5 years depending on those factors.
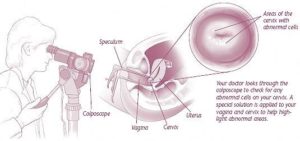
What is colposcopy?
If your Pap test is abnormal or the HPV screen is positive, repeat testing may be recommended. Or you may be asked to schedule a colposcopy.
This procedure is done in the office and is actually quite simple. During a pelvic exam, a high powered microscope is used to look more closely at your cervix. With a special solution, abnormal cells stand out from the surrounding normal cells and targeted biopsies of the abnormal areas are done. These biopsies are relatively pain free and no anesthesia is required.
The biopsies are sent to the laboratory where a Pathologist can determine the level of abnormality present within the cells of the cervix. These abnormalities are “graded” as normal, grade 1, grade 2, grade 3 or invasive cancer. Grades 1 through 3 are known as cervical intraepithelial neoplasia or “CIN.”
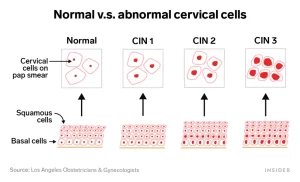
The risk for cancer increases as the level of abnormality of the cells increases. The risk of developing cervical cancer is 1% with a CIN 1 biopsy, whereas 12-40% of women with a CIN 3 biopsy will progress to cancer if left untreated. Follow up recommendations may include repeat testing with pap smear or treatment with an excision or ablative procedure.

